Juan P. Simone, MD
Philipp N. Streubel, MD
Joaquín Sánchez-Sotelo, MD
Scott P. Steinmann, MD
Julie E. Adams, MD
Abstract
Introduction: The purpose of this study was to investigate whether a safe zone rule could be applied to prevent iatrogenic injuries to the radial nerve (RN); and determine whether there is a relationship between the diameter of the radial head and capitellum and the distance of the posterior interosseous nerve (PIN) to the radiocapitellar joint.
Methods: Ten fresh-frozen cadaveric specimens were used to measure the distances between the RN and the lateral epicondyle; the PIN and the radiocapitellar joint; the lateral epicondyle and the PIN as it crossed the ulnohumeral joint; the diameter of the radial head; the width of the capitellum; and the fingerbreadths of the specimens.
Results: Four fingerbreadths determined a safe zone between the lateral epicondyle and the RN proximally at the point at which it pierced the intermuscular septum and the mid-lateral portion of the humeral shaft. Two fingerbreadths provided a safe zone for the
PIN from the radiocapitellar joint to the midpoint of the axis of the radius only with the forearm in pronation.
Conclusion: A four-finger rule, two-finger rule, and radial head diameter or capitellum size may predict a safe zone for the RN and PIN except for the segment of the nerve where it crosses the anterior cortex of either the humerus or radius.
Level of Evidence: Preclinical cadaveric study
Lateral approaches are commonly used for trauma and reconstructive cases around the elbow. The radial nerve (RN) is at particular risk at the distal humerus while placing external fixator pins, intramedullary blocking screws, and in lateral extended approaches.1–3 Surgical procedures involving the radial head and neck require special precaution to avoid posterior interosseous nerve (PIN) lesions.4–10 Precise anatomic knowledge of the nerve’s path is essential to avoid iatrogenicinjuries.2,9,11,12 Injuries may be sustained by direct trauma or indirectly by soft-tissue retraction, impingement of instrumentation, or suture.13,14 The RN pierces the lateral intermuscular septum of the arm and lateral border of the humerus from posterior to anterior at an average range of 10.2 to 12.5 cm proximal to the lateral epicondyle.2,11,12 The PIN courses along the anterior aspect of the radial neck; it is located 2.5 to
6.2 cm distal to the radial head depending on position forearm rotation upon different reports.2,6,7,11,15
Strategies to avoid iatrogenic RN injury during surgery include avoiding dissection too far proximally in the area of the nerve or alternatively definitive identification of the RN and protection. Typically, the authors use the technique described by Gerwin et al16 for extensile proximal approaches, in which the posterior cutaneous nerve of the arm is identified and traced proximally to its origin from the RN proper.
Strategies to avoid iatrogenic PIN injury include limiting the distal extent of the surgical approach and positioning the forearm in pronation or alternatively, identification and protection of the PIN by dissection of the supinator brevis muscle.6,10,13,17 Pronating the forearm increases safe exposure by moving the nerve anteriorly and more parallel to the radial shaft.3,5–7,9,12,17,18 The shortest distance from the radiocapitellar joint to the PIN with the forearm in pronation ranged between 2.9 and 4.5 cm. in different studies5–7 This considerable difference makes it difficult to predict a safe zone for surgery without risk of nerve injury. Distance variation may be due to different measurement techniques used and also because of different forearm sizes within patients or cadavers.
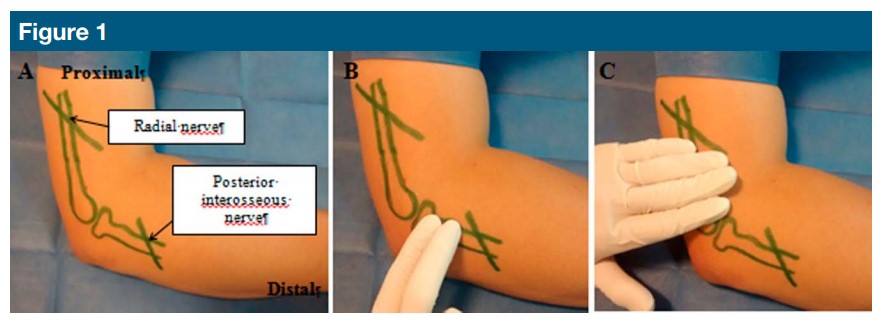
Photographs showing skin markings of lateral epicondyle, radial head, radial nerve, and posterior interosseous nerve (A) to demonstrate the two-finger rule (B) and four-finger rule (C).
The authors of this study use the two- and four-finger rule to delineate a safe zone for the RN and the PIN: Two fingerbreadths distal to the radial head to protect the PIN (twofinger rule) and four fingerbreadths proximal from the lateral epicondyle for the radial nerve (four-finger rule).
In the four-finger rule, the surgeon applies his fingers to the lateral aspect of the humerus, placing the hand at the lateral epicondyle, then measuring the width of the four fingers proximally to delineate a safe zone
for surgery without risk to the RN.
The two-finger rule is applied by the surgeon placing his hand on the proximal lateral forearm at the radiocapitellar joint, and measuring the width of the index and long finger (ie, the “two fingers”) distally to define a safe zone to avoid injury to the PIN (Figure 1).
Certainly, the surgeon’s own hand represents a constant for him, whereas the size of the patient’s arm represents a variable throughout cases. We therefore propose to correlate the size of the patient’s own fingers with the safe zones for surgery of the RN
and PIN versus the two- and fourfinger rules in this cadaver study.
The purpose of this study is to: (1) determine whether the two- and four finger rule is a reliable and reproducible method of determining a safe zone for the RN and PIN, (2) measure the distance of the RN from the lateral epicondyle at three different sites
along the distal humerus where it might be injured during surgery, (3) measure the distance of the PIN from the radiocapitellar joint and lateral epicondyle at three different locations where it might be injured during surgery, and (4) determine whether there is a relationship between the diameter of the radial head and capitellum and the distance of the PIN to the radiocapitellar joint.
Methods
Ten fresh-frozen cadaveric specimens consisting of the entire upper extremity from the medial border of
the scapula to the hand and fingers were obtained with Institutional Review Board approval through our
tissue repository. There were two right and eight left upper extremities from four female and six male specimens with a mean age at the time of death of 82 years (range, 59 to 103). No elbows had previous trauma that could interfere with accurate dissection and measurements.
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Simon, Dr. Streubel, Dr. Sánchez-Sotelo, and Dr. Steinmann, and Dr. Adams.
A lateral approach extending from the distal half of the arm down to the lateral epicondyle was performed in all specimens. Careful dissection between the anterior and posterior compartment was done to reveal the RN from where it pierced the intermuscular septum to the medial border of the brachioradialis muscle. A single investigator used a Vernier digital caliper (error 60.002 mm) to take measurements using two decimal places. The distance between the most prominent point of the lateral epicondyle and the RN as it emerged from the intermuscular septum, anterior border of the humerus, and mid-lateral portion of the humeral shaft (three distinct locations where the RN might be damaged during surgery) was taken (Figure 2). The width of the index, middle, ring, and small fingers (four fingerbreadths) along the proximal interphalangeal joints of the same cadaveric specimen were measured to assess whether the four-finger rule would apply to any of the three distances described earlier.
The approach was then extended distally to the proximal third of the forearm. Deeper dissection was performed simulating an anterior column approach extending it through an extensor digitorum splitting approach.19 The supinator muscle was carefully split and the PIN was visualized as it crossed the lateral aspect of the proximal radius. The distance between the midpoint of the radiocapitellar joint and the PIN as it crossed the anterior cortex of the proximal radius (where retractor placement might damage the nerve) and midpoint of the axis of the radius (where direct injury from dissection could damage the nerve) were measured in positions of both full pronation and full supination.
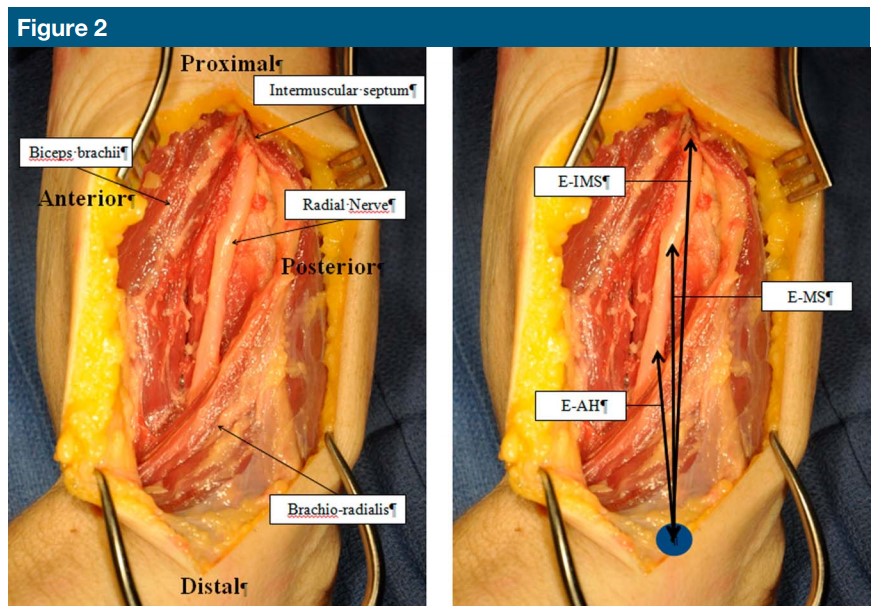
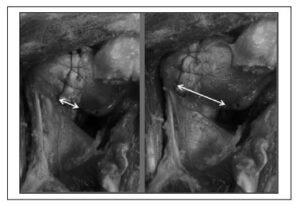
Photographs showing radial nerve dissection (left) and measurements (right). EAH = epicondyle to anterior humeral cortex distance, E-IMS = epicondyle to intermuscular septum distance, E-MS = epicondyle to the midportion of the humeral shaft distance
The distance between the lateral epicondyle and the PIN as it crossed the ulnohumeral joint medially was also measured (where it might be damaged from retraction or dissection while releasing the anterior capsule) (Figure 3).
The width of one and two fingerbreadths (index and long fingers) of the same specimen was measured at the distal interphalangeal joint level to assess whether the two-finger rule would apply to any of the two measurements of the PIN at the radius either in supination or pronation.
Finally, the diameter of the radial head in pronation and supination and the width of the capitellum in the sagittal plane were measured as well to see whether there was a relationship between these and the PIN safe zone.
Statistical Analyses
Descriptive statistics included means and ranges for continuous data.
Univariate linear regression was used to assess associations between radial head diameter, capitellum size, fingerbreadths, and RN and PIN distances. Statistical significance was set at P value less than 0.05.
Results
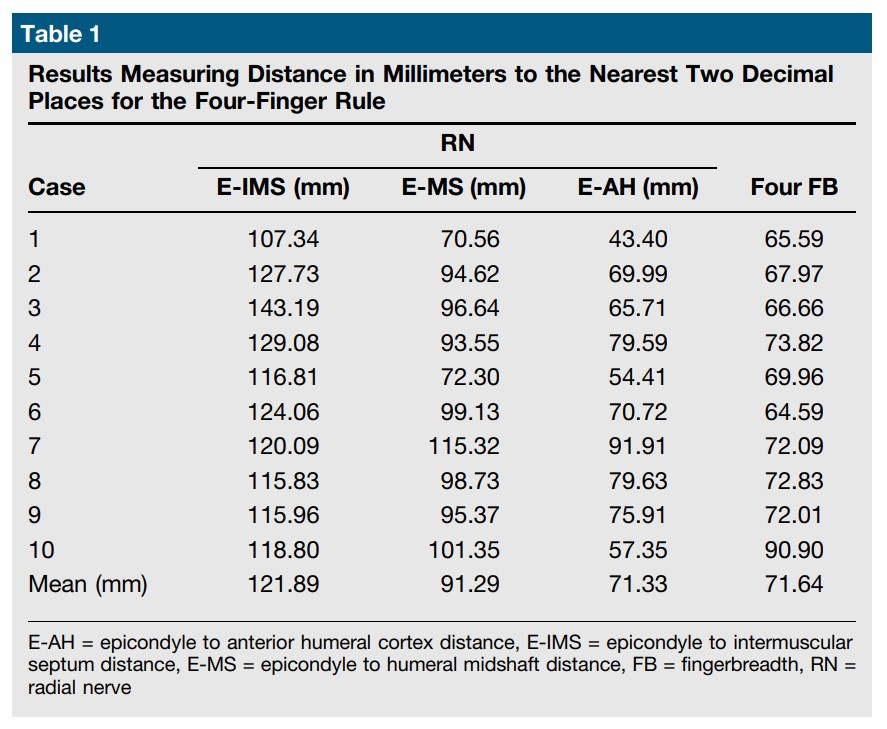
The mean distances between the lateral epicondyle and the RN proximally at the three sites of interest (point at which it pierces the intramuscular septum, at the mid-lateral portion of the shaft, and at the anterior humeral cortex) are summarized in Table 1.
This demonstrated that the fourfinger rule determined a safe zone for most of the measurements. It was not safe for four cases in which fourfingerbreadth distance was shorter than the distance of the lateral epicondyle to the RN as it crossed the anterior cortex of the humeral shaft.
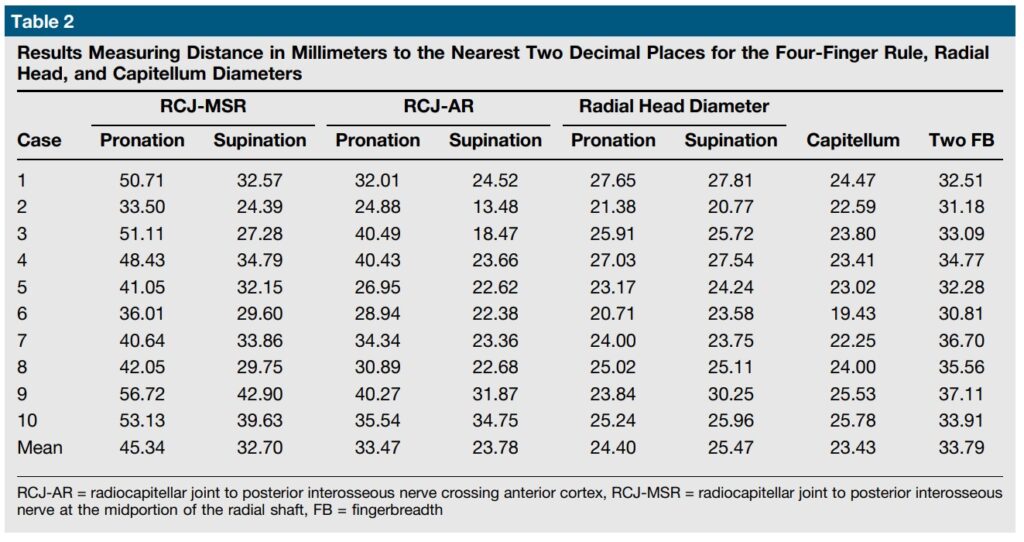
The distances between the radiocapitellar joint and the PIN as it crossed the anterior cortex of the proximal radius and midpoint of the axis of the radius are summarized in Table 2.
Only with the forearm in pronation did the two-fingerbreadth distance provide a safe zone for the PIN crossing the midpoint of the axis of the radius. The two-fingerbreadth distance did not determine a safe zone with respect to the PIN crossing the anterior cortex regardless of forearm position or the midpoint of the axis of the radius with the forearm in supination. The distance from the lateral epicondyle to the PIN as it crossed the ulnohumeral joint averaged 37.72 mm. (range, 31.61 to 44.72 mm).
Taking the diameter of the radial head or width of the capitellum would provide a safe zone to the PIN for all cases except for the PIN as it crosses the anterior cortex of the radial shaft in supination (Table 2).
There was a trend toward an increase in the distance of the PIN to the radiocapitellar joint with an increase of the size of the radial head and capitellum width that was statistically notable for the following cases: the PIN crossing the midpoint of the axis of the radius with the forearm in pronation (P = 0.03) and supination (P = 0.02) with the radial head diameter measured in supination; the PIN as it crossed the anterior cortex with the forearm in supination and the capitellum diameter (P = 0.01); the PIN as it crossed the anterior cortex with the forearm in supination and radial head diameter measured in supination (P = 0.03).
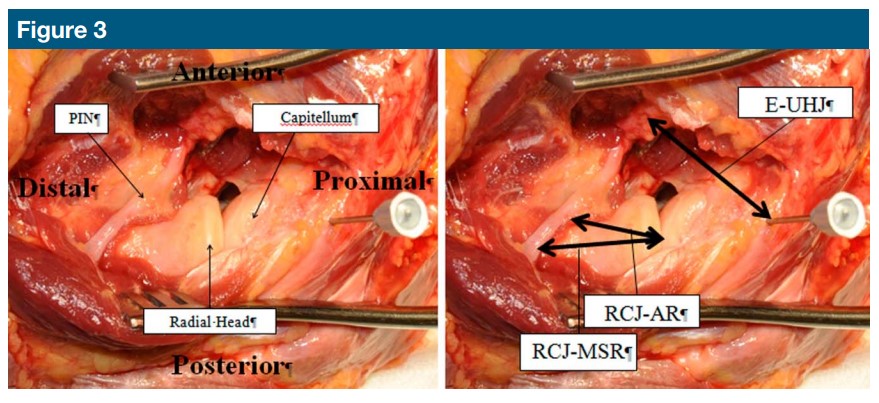
Photographs showing PIN dissection (left) and distances measured (right). EUHJ = epicondyle to ulnohumeral joint distance, PIN = posterior interosseous nerve, RCJ-AR = radiocapitellar joint to posterior interosseous nerve crossing anterior cortex, RCJ-MSR = radiocapitellar joint to posterior interosseous nerve at the midportion of the radial shaft
Discussion
Several studies have measured the distances from different landmarks to the RN or PIN with a wide range of variability across series.2,6,7,9,11 Intuitively, it seems that it would not be safe to consider a standardized safe zone distance for every different individual as these lengths do vary across series but also according to the relative size of the arm. Moreover, it is also important to point out the fact that these distances will vary not only according to forearm position but also to which segment of the bone the nerve is being measured.
In this study, we determined fixed parameters, such as two and four fingerbreadths and the diameter of the radial head or capitellum width to serve as guides to determine a safe zone for the PIN and RN. As both the RN and PIN have an oblique trajectory along the lateral humerus and radius, we measured different sites where these nerves might be damaged either directly or indirectly during surgical procedures. We also measured the average distance of the PIN from lateral epicondyle as it crosses the ulnohumeral joint to prevent injury when deeper dissection to the anterior capsule is needed. We have not found this distance reported before. It might be of interest to surgeons, specially while working on the anterior capsule during soft-tissue releases for stiff elbows.
The four-finger rule may be applied as a safe zone rule for the RN at the intermuscular membrane and midlateral portion of the humerus. While using this rule, the RN may be injured along the anterior cortex of the humerus because this distance is shorter than that where the nerve crosses the intermuscular septum or mid-lateral portion of the humerus.
Clement et al1 investigated RN injury caused by simulated percutaneous placement of external fixator half pins in humerus in a cadaver study. A direct injury to the nerve was observed in 4 of 40 placed half pins. In a study using 70 cadavers, Kamineni et al,2 suggested that the transepicondylar distance projected proximally along the lateral humeral shaft, from the lateral epicondyle, defines the absolute safe zone for pin placement. The authors suggest that inter-individual variations can be taken into account with this technique. Based on the results of our study, we would advise surgeons that sliding over the anterior cortex or aiming the pin anteriorly while placing distal humerus pins or blocking screws should be avoided because the RN is closer to the epicondyle in this area.
The two-fingerbreadth rule only provides a safe zone for the PIN crossing the midpoint of the axis of the radius with the forearm in pronation. Caution should be taken with this technique as the nerve was less than 2 mm distal to the twofingerbreadth measurement from the radiocapitellar joint even with the arm in pronation in one case. The twofingerbreadth distance does not determine a safe zone with respect to the PIN crossing the anterior cortex. Using the radial head diameter or capitellum width as a parameter determined a safe working area in every case except for the anterior cortex of the radius while the forearm was in supination.
PIN palsy after elbow surgery is a dreaded complication. Most of the time it is transient, which suggests that it may be caused by traction.13,14,20,21 If the nerve is not directly seen on the surgical field, gentle traction must be applied while retractors are placed on the anterior cortex of the radius.
An absolute safe zone for the PIN has not been determined yet. What we do know for sure is that forearm pronation increases the PIN safe zone area of the proximal radius from a lateral approach.3,5–7,9,12,17,18
In 2010, Cox et al11 reported that the PIN crossed the radial neck at an average of 10% of the radius’s complete length. This relationship gives us a more precise estimate of an individual’s PIN location according to the radial length. In the same study, the distance between the lateral epicondyle and the RN at the intermuscular septum averaged 38% of the humeral length.
In our study, we were able to determine that in most cases as the radial head diameter and capitellum size increases, so does the distance of the PIN to the radiocapitellar joint. We have found this as an association, but not as a correlation to predict the exact distance where the nerve would cross the radial neck. We have not found the same association regarding fingerbreadths and RN and PIN distances.
This might probably be because of soft tissue variations surrounding interphalangeal joints.
Limitations to our series are related to the cadaveric nature of our study.
First, we took measurements on cadaveric specimens where there was no elbow trauma. During surgical approaches in the injured elbow, the normal anatomy and relationships are often altered by the trauma. Second, the fact that measurements were made on fresh frozen cadaveric fingers would also likely give a smaller value that what would be expected in a living patient, due to loss of soft tissue turgor. Third, the length of one’s finger may be related to his or her stature. The width of their fingers may vary according to their occupation or other factors. We do not know the previous occupation that the cadavers were involved in to draw further conclusions.
Calfee et al15 showed in a cadaveric study simulating forearm trauma that after an osteotomy, the position
of the PIN was largely unaffected by forearm rotation and that radial head excision and proximal migration of the radius resulted in the PIN crossing the radius closer to the radiocapitellar joint across all forearm positions. In addition, in a cadaver specimen, muscle tension is not the same as in a surgical patient where the measured distances might be slightly modified from the ones measured.
Conclusion
When exposing the distal humerus or proximal radius with a posterolateral exposure, careful nerve dissection is the best way to avoid iatrogenic injuries. While doing percutaneous procedures to the distal humerus or limited exposures on the proximal radius, the four-finger rule, twofinger rule, and radial head diameter or capitellum size may predict a safe zone for the RN and PIN except for the segment of the nerve where it crosses the anterior cortex of each bone. Special precaution should be taken while placing anterior retractors to avoid traction injuries.
A larger diameter of the radial head and larger capitellum size is associated with larger PIN safe zones but does not guarantee it. Our series, concordant with previous studies, demonstrates that pronation will always increase the PIN safe zone area when using a lateral approach to the radial head.
Acknowledgment
The authors wish to thank the donors and the family of the donors used for this research.
References
1. Clement H, Pichler W, Tesch NP, Heidari N, Grechenig W: Anatomical basis of the risk of radial nerve injury related to the technique of external fixation applied to the distal humerus. Surg Rad Anat 2010;32: 221-224.
2. Kamineni S, Ankem H, Patten DK: Anatomic relationship of the radial nerve to the elbow joint: Clinical implications of safe pin placement. Clin Anat 2009;22: 684-688.
3. Noger M, Berli MC, Fasel JH, Hoffmeyer PJ: The risk of injury to neurovascular structures from distal locking screws of the unreamed humeral nail (UHN): A cadaveric study. Injury 2007;38:954-957.
4. Adams JE, Steinmann SP: Nerve injuries about the elbow. J Hand Surg Am 2006;31: 303-313.
5. Diliberti T, Botte MJ, Abrams RA: Anatomical considerations regarding the posterior interosseous nerve during posterolateral approaches to the proximal part of the radius. J Bone Joint Surg Am 2000;82:809-813.
6. Laton JN, Cameron-Donaldson M, Blazar PE, Moore JR: Anatomic considerations regarding the posterior interosseous nerve at the elbow. J Shoulder Elbow Surg 2007; 16:502-507.
7. Schimizzi A, MacLennan A, Meier KM, Chia B, Catalano LW III, Glickel SZ: Defining a safe zone of dissection during the extensor digitorum communis splitting approach to the proximal radius and forearm: An anatomic study. J Hand Surg Am 2009;34:1252-1255.
8. Strauch J, Rosenwasser MP, Glzer PA: Surgical exposure of the dorsal proximal third of the radius: How vulnerable is the posterior interosseous nerve? J Shoulder Elobw Surg 1996;5:342-346.
9. Vergara Amador E: Anatomic aspects of the posterior interosseous nerve in the proximal approach to the radius. Acta Orthop Mex 2008;22:309-315.
10. Witt JD, Kamineni S: The posterior interosseous nerve and the posterolateral approach to the proximal radius. J Bone Joint Surg Br 1998;80:240-242.
11. Cox CL, Riherd D, Tubbs RS, Bradley E, Lee DH: Predicting radial nerve location using palpable landmarks. Clin Anat 2010; 23:420-426.
12. Heidari N, Kraus T, Weinberg AM, Weiglein AH, Grechenig W: The risk injury to the posterior interosseous nerve in standard approaches to the proximal radius: A cadaver study. Surg Rad Anat
2011;33:353-357.
13. Tornetta P III, Hochwald N, Bono C, Grossman M: Anatomy of the posterior interosseous nerve in relation to fixation of the radial head. Clin Orthop Relat Res 1997;345:215-218.
14. Van Geertryden PG: Iatrogenic posterior interosseous nerve palsy following an elbow fracture. Acta Orthop Belg 1996;64:221-224.
15. Calfee RP, Wilson JM, Wong HW: Variations in the anatomic relations of the posterior interosseous nerve associated with proximal forearm trauma. J Bone Joint Surg Am 2011;93:81-90.
16. Gerwin M, Hotchkiss RN, Weiland AJ: Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial
nerve. J Bone Joint Surg Am 1996;78: 1690-1695.
17. Strachan CH, Ellis BW: Vulnerability of the
posterior interosseous nerve during radial head resection. J Bone Joint Surg Br 1971; 53:320-323.
18. Kaplan EB: Surgical approach to the proximal end of the radius and its use in fractures of the head and neck of the radius. J Bone Joint Surg 1941;23:86-92.
19. Ring D, King D: Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability. Surgical technique. J Bone Joint Surg Am 2008; 90(suppl 2 pt 1):63-73.
20. Mekhail AO, Ebraheim MA, Jackson WT, yeasting RA: Vulnerability of the posterior interosseous nerve during proximal radius exposures. Clin Orthop Relat Res 1995; 315:199-208.
21. Nigro PT, Cain R, Mighell MA: Prognosis for recovery of posterior interosseous nerve palsy after distal biceps repair. J Shoulder Elbow Surg 2013;22:70-73.