Juan Pablo Simone 1, Philipp N. Streubel 2, Joaquin Sanchez-Sotelo 3, Scott P. Steinmann 3, and Julie E. Adams 3,4
Abstract
Background: This study investigated whether axillary nerve (AN) distance to the inferior border of the humeral head and inferior glenoid would change while placing the glenohumeral joint in different degrees of external rotation and abduction.
Methods: A standard deltopectoral approach was performed on 10 fresh-frozen cadaveric specimens. The distance between AN and the inferior border of the humeral head and inferior glenoid while placing the shoulder in 0°, 45°, and 90° of external rotation or abduction was measured. Continuous variables for changes in AN position were compared with paired 2-tailed Student t test. Results: The mean distance between the AN and the humeral head with the shoulder in 0°, 45°, and 90° of external rotation and 0° of abduction was 13.77 mm (SD 4.31), 13.99 mm (SD 4.12), and 16.28 mm (SD 5.40), respectively. The mean distance between the AN and glenoid with the shoulder in 0°, 45°, and 90° of external rotation was 16.33 mm (SD 3.60), 15.60 mm (SD 4.19), and 16.43 (SD 5.35), respectively. The mean distance between the AN and the humeral head with the shoulder in 0°, 45°, and 90° of abduction and 0° of external rotation was 13.76 mm (SD 4.31), 10.68 mm (SD 4.19), and 3.81 mm (SD 3.08), respectively. The mean distance between the AN and glenoid with the shoulder in 0°, 45°, and 90° of abduction was 16.33 mm (SD 3.60), 17.66 mm (SD 5.80), and 12.44 mm (SD 5.57), respectively. Conclusions: The AN position relative to the inferior aspect of the glenohumeral joint does not significantly change despite position of external rotation. Increasing shoulder abduction over 45° decreases the distance from the glenohumeral joint to the AN and should be avoided.
Keywords: axillary nerve, glenohumeral joint, shoulder abduction, shoulder external rotation, deltopectoral approach
Introduction
The axillary nerve (AN) is the most common peripheral nerve injured during shoulder surgery.17,19 Although care is taken to avoid iatrogenic injury, the AN is at particular risk in any surgery that involves the deltopectoral approach at
the anteroinferior aspect of the glenohumeral joint or during a deltoid split approach at a distance of 4 to 6 cm from the acromion.7,17 In particular, subscapularis tenotomy and anterior capsulotomy are commonly used in the setting of shoulder replacement surgery and for open anterior instability. While performing this procedure, the AN is vulnerable to injury as it may be as close as 3 mm from the inferior glenohumeral capsule.2,14
Precise anatomic knowledge of the nerve’s path is essential to avoid iatrogenic injury.1,12,18 The AN runs obliquely across the inferolateral border of the subscapularis and enters the quadrilateral space. It divides into an anterior and posterior branch. The posterior branch innervates the teres minor muscle and the posterior deltoid muscle; it then terminates as the superior lateral brachial cutaneous nerve.
The anterior branch travels deep in the deltoid fascia toward the anterior border of this muscle.6,9,17 Injuries of the AN may be sustained by a variety of means, including direct laceration or indirectly by soft tissue retraction, suture misplacement, impingement of instrumentation, stretching and positioning of the upper extremity.1,4,10,11,16 The prognosis of recovery depends on the severity of the nerve injury.
To protect the AN during an anterior approach to the glenohumeral joint such as for shoulder replacement or open instability repairs, external rotation and adduction of the glenohumeral joint are ecommended to increase the “safe zone.” External rotation may increase the distance between the AN and the subscapularis while performing a subscapularis tenotomy by reducing tension on the nerve and allowing it to fall away from the surgical field at the intended tendinous or capsular incision.13,17,22 With external rotation, the lesser tuberosity drives away from the AN making the tenotomy or capsulotomy safer (Figure 1).
1 Shoulder and Elbow Surgery, Hospital Alemán, Buenos Aires, Argentina
2 Shoulder, Elbow and Hand Surgery, Department of Orthopedic Surgery,
University of Nebraska Medical Center, Omaha, USA
3 Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN, USA
4 Department of Orthopedic Surgery, Mayo Clinic Health System, Austin, MN, USA
Corresponding Author: Julie E. Adams, Department of Orthopaedic Surgery, Mayo Clinic, 200 First Street, SW, Rochester, MN 55905, USA. Email: adams.julie@mayo.edu

Figure 1. Distance (marked with arrows) from the axillary nerve to tenotomy site (tagged with sutures) in 0° of external rotation (left) will increase while performing external rotation 90°(right).
Note. Notice that the position of the axillary nerve remains unchanged in both pictures. (Picture taken from a cadaver as a pilot dissection to this study.)
Several anatomic studies show detailed measurement
and relationship between the acromion and the AN.3,5,7,8,19
Cheung et al7 studied the effects of shoulder position on AN positions during the split lateral deltoid approach. This study showed the distance of the AN varies to the acromion depending on shoulder position and that shoulder abduction had the greatest effect on AN position.
To our knowledge, this same effect has not been studied for position of the AN at the inferior border of the humeral head and glenoid during a deltopectoral approach.
The purpose of this study is to quantify AN distance to
the inferior border of the humeral head and inferior glenoid during a deltopectoral approach and subscapularis tenotomy and to study the effect of altering external rotation and abduction upon the AN.
Materials and Methods
Ten fresh-frozen cadaveric specimens consisting of the entire upper extremity from the medial border of the clavicle to the hand and fingers were obtained with institutional review board approval through our tissue repository. There were 2 right and 8 left upper extremities from 4 female and 6 male specimens with a mean age at the time of death of 82 years (range, 59-103 years). No shoulders had previous upper limb
trauma or significant injury or history of surgery, which could interfere with accurate dissection and measurements.
Dissection was carried out using a deltopectoral approach on the 10 cadavers. An anterior arthrotomy was done through a subscapularis tenotomy. The AN was dissected and exposed.
The closest distance between the 6-o’clock position of the inferior border of the glenoid and inferior border of the humeral head to the closest point of the AN was measured using a Vernier digital caliper (error ±0.002 mm) rounded to the nearest 2 decimal places with the shoulder at 0° of external rotation and abduction (Figure 2). This was then repeated with the shoulder in 45° and 90° of external rotation and abduction separately to see if there was any significant change in nerve position according to shoulder position.
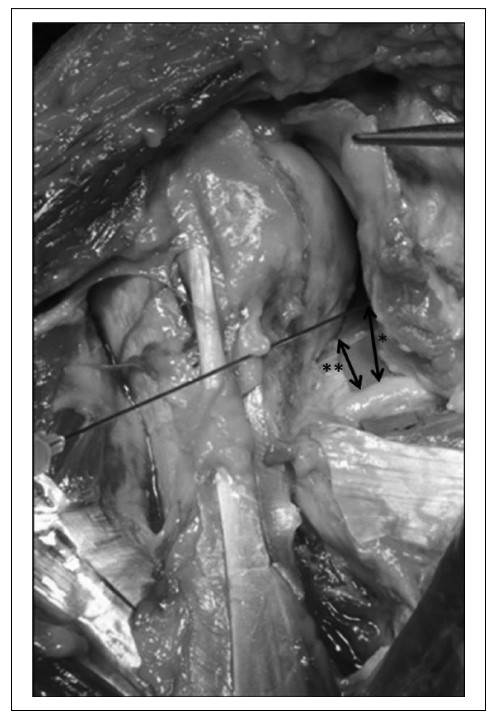
Figure 2. Measurement taken for the closest distance between the axillary nerve and the inferior border of the glenoid at the 6-o’clock position (*) and the inferior border of the humeral head (**) at 0° of external rotation and abduction.
For accurate measurement of glenohumeral position, the upper extremity was held flat on the dissection table. Zero degrees of external rotation were set with the elbow joint at 90° of flexion and perpendicular to the plane of the dissection table. Forty-five degrees and 90° of external rotation were then measured while rotating the hand away from the specimen while keeping the shoulder at 0° of abduction. Zero degrees of abduction were set with the humeral shaft parallel to the medial border of the scapula. Forty-five degrees and 90° of abduction were measured while separating the elbow from the axis of the upper extremity.
Statistical Analyses
Descriptive statistics included means, standard deviation, and ranges for continuous data. Continuous variables for changes in AN position were compared with paired 2-tailed Student t test. Statistical significance was set at P value less than .05.
Results
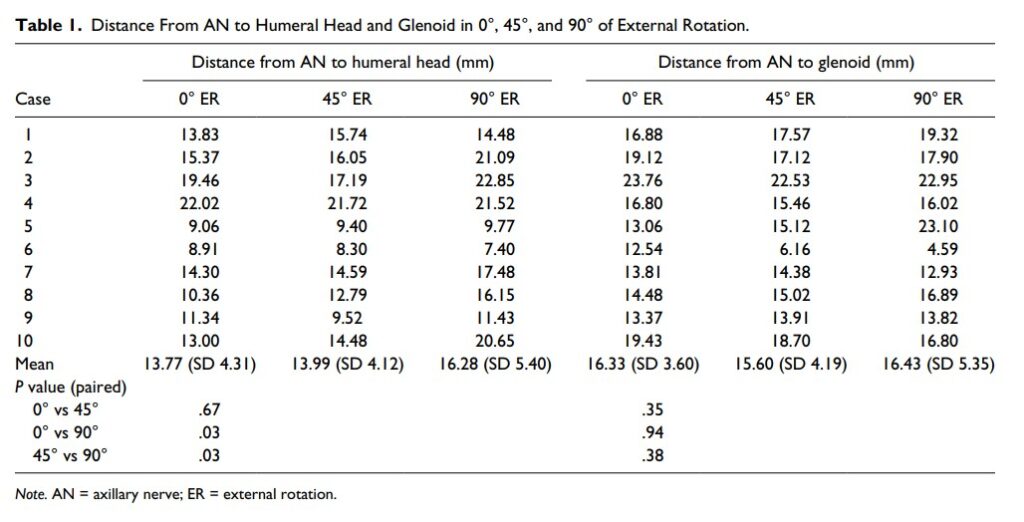
The mean distance between the AN and the humeral head with the shoulder in 0°, 45°, and 90° of external rotation and 0° of abduction was 13.77 mm (SD 4.31; range 8.91-22.02), 13.99 mm (SD 4.12; range 8.30-21.72), and 16.28 mm (SD 5.40; range 7.40-22.85), respectively. The P paired value for 0° vs 45°, 0° vs 90°, and 45° vs 90° was .67, .03, and .03, respectively. The mean distance between the AN and glenoid with the shoulder in 0°, 45°, and 90° of external rotation was 16.33 mm (SD 3.60; range 12.54-23.76), 15.60 mm (SD 4.19; range 6.16-22.53), and 16.43 mm (SD 5.35; range 4.59-23.10), respectively. The P paired value for 0° vs 45°, 0° vs 90°, and 45° vs 90° was .35, .94, and .36, respectively (Table 1).
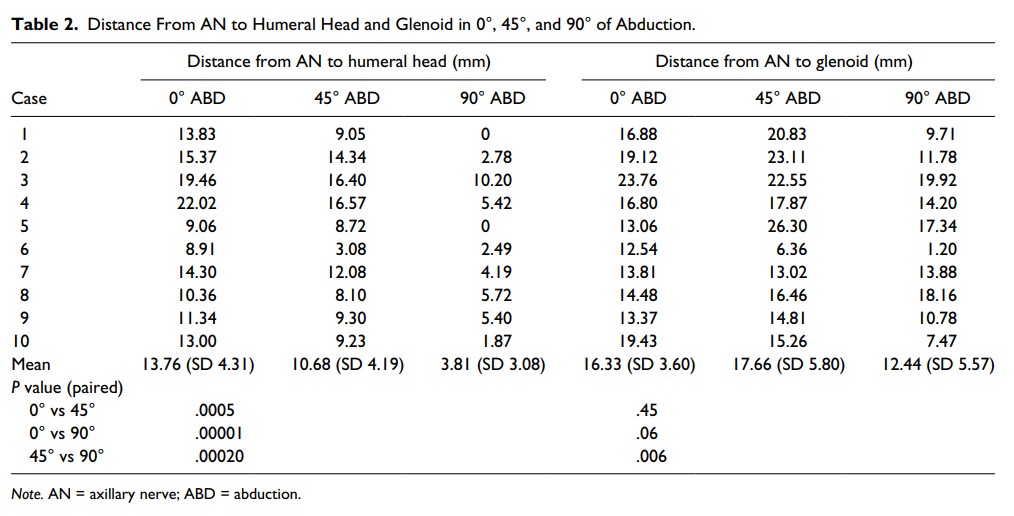
The mean distance between the AN and the humeral head with the shoulder in 0°, 45°, and 90° of abduction and 0° of external rotation was 13.76 mm (SD 4.31; range 8.91-22.02), 10.68 mm (SD 4.19; range 3.08-16.57), and 3.81mm (SD 3.08; range 0-10.20), respectively. The P pairedvalue for 0° vs 45°, 0° vs 90°, and 45° vs 90° was .0005, .00001, and .0002, respectively. The mean distance between the AN and glenoid with the shoulder in 0° of external rotation, 45° and 90° of abduction was 16.33 mm (SD 3.60; range 12.54-23.76), 17.66 mm (SD 5.80; range 3.36-26.30), and 12.44 mm (SD 5.57; range 1.20-19.92), respectively.
The P paired value for 0° vs 45°, 0° vs 90°, and 45° vs 90° was .45, .06, and .006, respectively (Table 2).
Discussion
The incidence of neurologic injury after anterior shoulder surgery such as shoulder replacement and anterior instability procedures ranges from 1% to 8.2 % and is probably underreported.10,14,20 The primary mechanism of nerve injury is traction affecting mainly the posterior and lateral chords of the brachial plexus.10,14,16 Nagda et al16 assessed peripheral nerve function during shoulder arthroplasty with electrodiagnostic studies. In this study, 50% of the nerve events (sustained neurotonic electromyographic activity or greater than 50% amplitude reduction in the transcranial electrical motor evoked potentials from 1 or more muscles) occurred while the patient’s shoulder was positioned in abduction, external rotation, and extension. Thirty-seven percent occurred in adduction, external rotation, and extension. Thirteen percent occurred while the shoulder was placed in abduction with the elbow was in at least 90° of flexion.
Laderman et al11 assessed the prevalence of subclinical neurologic lesions following reverse shoulder arthroplasty and compared it with the prevalence after anatomic shoulder arthroplasty. Postoperatively, electromyography revealed acute lesions involving mainly the AN in 9 out of 19 shoulders with a reverse replacement. Eight of the 9 shoulders completely resolved at 6 months by electromyographic examination. One of 23 shoulders in the anatomic shoulder arthroplasty group presented with acute postoperative neurologic lesions confirmed by electromyography. At 12 months follow-up, this patient still had incomplete recovery by electromyography.
Most lesions due to traction and position will produce a neurapraxia, which will eventually recover in time.11 Severe injuries (axonotmesis or neurotmesis) are most commonly caused by direct nerve injuries, such as laceration or suture placement. These tend to be isolated terminal nerve branch injuries, which will require surgical management and have poorer prognoses. Carofino et al4 reported upon iatrogenic
nerve injuries following shoulder surgery in 26 patients.
Sixteen injuries were to a terminal nerve branch including the AN in 9 cases. Four cases resulted following open procedures to treat instability, 4 following isolated arthroscopic procedures, and 1 combined open and arthroscopic procedure. The mechanisms of injury involved nerve laceration and suturing of the nerve to the capsule.
In our study, the distance between the AN and the inferior border of the humeral head changed its position significantly when comparing 0° to 90° and 45° to 90° of external rotation (P = .03). Rotating the arm externally up to 45° does not change the nerve position significantly. The distance from the AN to the humeral head also changed its position significantly while comparing 0° to 45°, 0° to 90°, and 0°to 45° (P = .005, .00001, and .0002) of abduction.
The distance between the AN and the inferior border of theglenoid changed significantly while comparing 45° to 90° (P = .006) of abduction.
Limited information is available in the current literature regarding the position of the AN relative to the glenohumeral joint and the effects of shoulder positioning in external rotation and shoulder abduction. Yoo et al21 studied the AN in relation to the glenoid and arm position from an arthroscopic perspective. The nerve was found closest to the
glenoid at the 5:30- to 6:00-o’clock position (right) or 6:00-to 6:30-o’clock position (left) being the closest distance range from 10 to 25 mm. In concordance with our findings, regardless of the arm position, the path of the nerve demonstrated little change with different arm positions.
In an anatomic study of the innervation of the inferior glenohumeral ligament, Gelber et al9 described that the articular neural branches of the AN, in the 4 specimens studied, relaxed and separated from the joint at 45° of external rotation and 60° of abduction; however, the change in position was not quantified.
Limitations to our series are related to the cadaveric nature of our study. We took measurements on cadaveric specimens where there was no degenerative joint disease or previous trauma. During surgical approaches in patients with osteoarthritis or instability, due to scar tissue or even previous surgeries, normal anatomy and relations are frequently changed. Decreased muscle tension in a cadaver may also contribute to altered relationship between the AN and bony structures. Small sample size and low power may also limit finding clinically important differences. However, our study was able to show a statistically significant change in position of the AN in several positions of both external rotation and abduction.
For this reason, we recommend careful identification of the location and course of the AN during anterior shoulder surgery. When splitting the anteroinferior capsule for means of shoulder stabilization or soft tissue release, the AN should be protected by placing a blunt retractor along the inferior aspect of the glenohumeral capsule, thereby shielding the nerve from iatrogenic injury. Dissection may be avoided when using a subscapularis muscle splitting approach in operations for anterior shoulder instability.
When done carefully, this technique can successfully allow exposure of the anterior and inferior capsule without requiring exposure or palpation of the AN.15
The AN position relative to the inferior aspect of the glenohumeral joint changes significantly while positioning the shoulder in different degrees of external rotation or abduction during surgery. However, external rotation will draw the lesser tuberosity away from the nerve making the tenotomy or capsulotomy safer. For this reason, external rotation is recommended in anterior shoulder surgery. Increasing shoulder abduction decreases the distance to the AN of and should be taken into account or avoided if instrumenting in the vicinity of the axillary nerve.
Acknowledgments
We thank the donors of the cadavers and their families for providing the materials needed to perform this study.
Ethical Approval
This study was approved by our institutional review board.
Statement of Human and Animal Rights
Procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Statement of Informed Consent
No informed consent was required (cadaver study).
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Scott P. Steinmann reports other from Arthrex, other from
Biomet, outside the submitted work.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported in part by a grant from Small Grants Program,
Mayo Foundation.
References
1. Apaydin N, Tubbs RS, Loukas M, Duparc F. Review of the surgical anatomy of the axillary nerve and the anatomic basis of its iatrogenic and traumatic injury. Surg Radiol Anat. 2010;32:193-201.
2. Boardman ND III, Cofield RH. Neurologic complications of shoulder surgery. Clin Orthop Relat Res. 1999;368: 44-53.
3. Burkhead WZ, Scheinberg RR, Box G. Surgical anatomy of the axillary nerve. J Shoulder Elbow Surg. 1992;1: 131-136.
4. Carofino BC, Brogan DM, Kircher MF, et al. Iatrogenic nerve injuries during shoulder surgery. J Bone Joint Surg Am. 2013;95:1667-1674.
5. Cetik O, Uslu M, Acar HI, Comert A, Tekdemir I, Cift H. Is there a safe area for the axillary nerve in the deltoid muscle? A cadaveric study. J Bone Joint Surg Am. 2006;88: 2395-2399.
6. Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy. 2008;24:689-696.
7. Cheung S, Fitzpatrick M, Lee TQ. Effects of shoulder position on axillary nerve positions during the split lateral deltoid approach. J Shoulder Elbow Surg. 2009;18:748-755.
8. Gardner MJ, Griffith MH, Dines JS, Briggs SM, Weiland AJ, Lorich DG. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res. 2005;434:123-129.
9. Gelber PE, Reina F, Monllau JC, Yema P, Rodriguez A, Caceres E. Innervation patterns of the inferior glenohumeral ligament: anatomical and biomechanical relevance. Clin Anat. 2006;19:304-311.
10. Ho E, Cofield RH, Balm MR, Hattrup SJ, Rowland CM. Neurologic complications of surgery for anterior shoulder instability. J Shoulder Elbow Surg. 1999;8:266-270.
11. Lädermann A, Lübbeke A, Mélis B, et al. Prevalence of neurologic lesions after total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93:1288-1293.
12. Liu KY, Chen TH, Shyu JF, Wang ST, Liu JY, Chou PH. Anatomic study of the axillary nerve in a Chinese cadaveric population: correlation of the course of the nerve with proximal humeral fixation with intramedullary nail or external skeletal fixation. Arch Orthop Trauma Surg. 2011;131:669-674.
13. Loomer R, Graham B. Anatomy of the axillary nerve and its relation to inferior capsular shift. Clin Orthop Relat Res. 1989;243:100-105.
14. Lynch NM, Cofield RH, Silbert PL, Hermann RC. Neurologic complications after total shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5:53-61.
15. McFarland EG, Caicedo JC, Kim TK, Banchasuek P. Prevention of axillary nerve injury in anterior shoulder reconstructions: use of a subscapularis muscle-splitting technique and a review of the literature. Am J Sports Med. 2002;30:601-606.
16. Nagda SH, Rogers KJ, Sestokas AK, et al. Neer Award 2005: peripheral nerve function during shoulder arthroplasty using intraoperative nerve monitoring. J Shoulder Elbow Surg. 2007;16(suppl 3):S2-S6.
17. Perlmutter GS. Axillary nerve injury. Clin Orthop Relat Res. 1999;368:28-36.
18. Steinmann SP, Moran EA. Axillary nerve injury: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:328-335.
19. Sung CM, Roh GS, Sohn HJ, et al. Prediction of the location of the anterior branch of the axillary nerve, using correlations with physical factors: a cadaveric study. J Shoulder Elbow Surg. 2013;22:e9-e16.
20. Wirth MA, Rockwood CA Jr. Complications of shoulder arthroplasty. Clin Orthop Relat Res. 1994;307:47-69.
21. Yoo JC, Kim JH, Ahn JH, Lee SH. Arthroscopic perspective of the axillary nerve in relation to the glenoid and arm position: a cadaveric study. Arthroscopy. 2007;23:1271-1277.
22. Zuckerman JD, Sajadi KR. Approach and exposure for primary total shoulder arthroplasty: glenoid and proximal humerus. In: Zuckerman JD, ed. Advanced Reconstruction Shoulder. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2007:497-506.